KeraNatural for the treatment of keratoconus
Allograft corneal ring treatment, also known as KeraNatural, is a newer type of corneal ring treatment that uses allograft tissue (donor tissue) to create a natural corneal ring. This type of treatment is considered advantageous as it is safer, organic, biological, reversible and adjustable compared to conventional corneal ring therapy.
One advantage of allograft corneal ring treatment is that it uses natural tissue instead of synthetic material, which can reduce the risk of complications such as infection, corneal melting or inflammation. Also, because allograft tissue is biologically compatible, the risk of rejection is low.
Another advantage of allograft corneal ring treatment is that it is reversible and adjustable. Unlike traditional corneal ring treatment, which requires removal of the plastic rings if the patient experiences problems or complications, allograft corneal ring treatment can be easily adjusted or removed as needed.
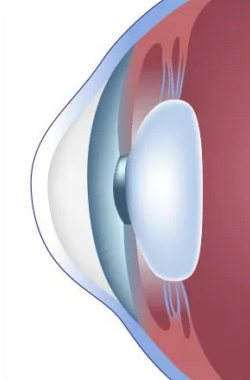
Normal cornea
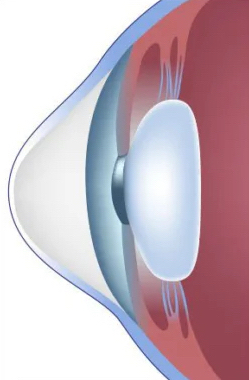
Keratoconus
However, it is important to remember that any surgical procedure carries risks and potential complications. Patients considering allograft corneal ring treatment should discuss the potential risks and benefits with their ophthalmologist or eye surgeon. Also, not all patients with keratoconus may be suitable candidates for corneal ring treatment and other treatment options may be necessary.
Frequently Asked Questions
Although the exact cause of this disease is unknown, it is believed that the greatest contributing factors are:
• a genetic predisposition via the inheritance of defective allels (genes)
• corneal trauma such as the one caused by the repetetive eye rubbing typical of allergic conjunctivitis.
The incidence of keratoconus varies in different parts of the world and it can be particularly high in cetain regions.
For the early diagnosis and treatment of the disease it is very important to carry out a detailed eye examination with Corneal Topography, especially in children with a family history of keratoconus.
Keratoconus most often starts during adolescence, although sometimes it could occur earlier. Patients typically are diagnosed in their 20s when the cornea becomes thinned and more curved than normal and the vision starts degrading. Generally the condition progresses between the ages of 20 and 40, and then it slows down or stops in the mid 40s.
• Failure to maintain clear vision despite frequent spectacle changes.
• Difficulty seeing clearly when driving, writing or reading.
• Wavy and diagonal view of straight lines.
• Contact lenses no longer fitting on the eye.
• Persistent itchy eyes, frequent allergies.
• Photosensitivity, glare when looking at the lights.
• Progression of myopia and astigmatism.
The presence of keratoconus may go unrecognized during routine eye examinations. A detailed eye examination with Corneal Topography is necessary to diagnose the disease.
These are the treatments currently available for progressive cheratoconus:
• EARLY STAGES with still good visual acuity: collagen cross linking to stabilize the disease and prevent further deterioration.
• INTERMEDIATE STAGES with reduced visual acuity and poor contact lens tolerance: possible indication for intra corneal rings surgery implantation (ICRS), either by means of a) traditional PMMA (plastic) rings or b) by a novel technique called CAIRS (corneal allogenic intrastromal ring segments implantation) in which strips of human donor cornea are implanted in the diseased cornea. The donor tissue that is implanted is called KeraNatural. The tissue can alternatively be prepared by the surgeon himself / herself using a donor cornea, but this is a lengthy procedure which carries a significant risk of infection and graft rejection.
• ADVANCED STAGES with severe corneal distrortion or scarring require corneal transplant, cheratoplasty (either deep anterior keratoplasty, DALK or penetrating keratoplasty, PK).
In certain cases collagen cross linking may be used in combination with ICRS or CAIRS and viceversa.
In selected cases, a topography-based PRK can be used simultaneously with collagen cross linking to shave off the tip of the cone and partially improve the quality of the vision.
KeraNatural is a completely biological method for reshaping the deforned cornea adding strenght to it without having to undergo a full corneal transplantation. This reduces astigmatism and also myopia and it improves the vision. Developed by the US Eye Bank, the KeraNatural method uses strips of human cornea. KeraNatural is placed in the tunnel created by the femtosecond laser in the cornea. The procedure takes approximately 10 minutes. No general anesthesia is administered to the patient during the procedure. The eyes are numbed with eye drops. The patient does not feel any pain and the next day can return to his/her normal life in a normal way.
The decision to use KeraNatural or cross-linking (or both) as treatment for keratoconus depends on the individual case and the severity of the condition.
Cross-linking is a non-invasive procedure that helps to strengthen the cornea and prevent further progression of keratoconus. It involves applying riboflavin drops to the cornea and then exposing the eye to UV (ultraviolet) light. This helps to increase the number of chemical bonds within the cornea, making it harder and more resistant to deformation.
KeraNatural instead involves implanting rings made of human cornea into the patient’s cornea to help reshaping it and improving vision.
I usually perform KeraNatural first and then apply crosslinking 6 months later to stabilize the corneas, but there is no harm in doing KeraNatural in patients who have already had crosslinking. This actually happens frequently because crosslinking is typically used as first line treatment in the early stages of keratoconus.
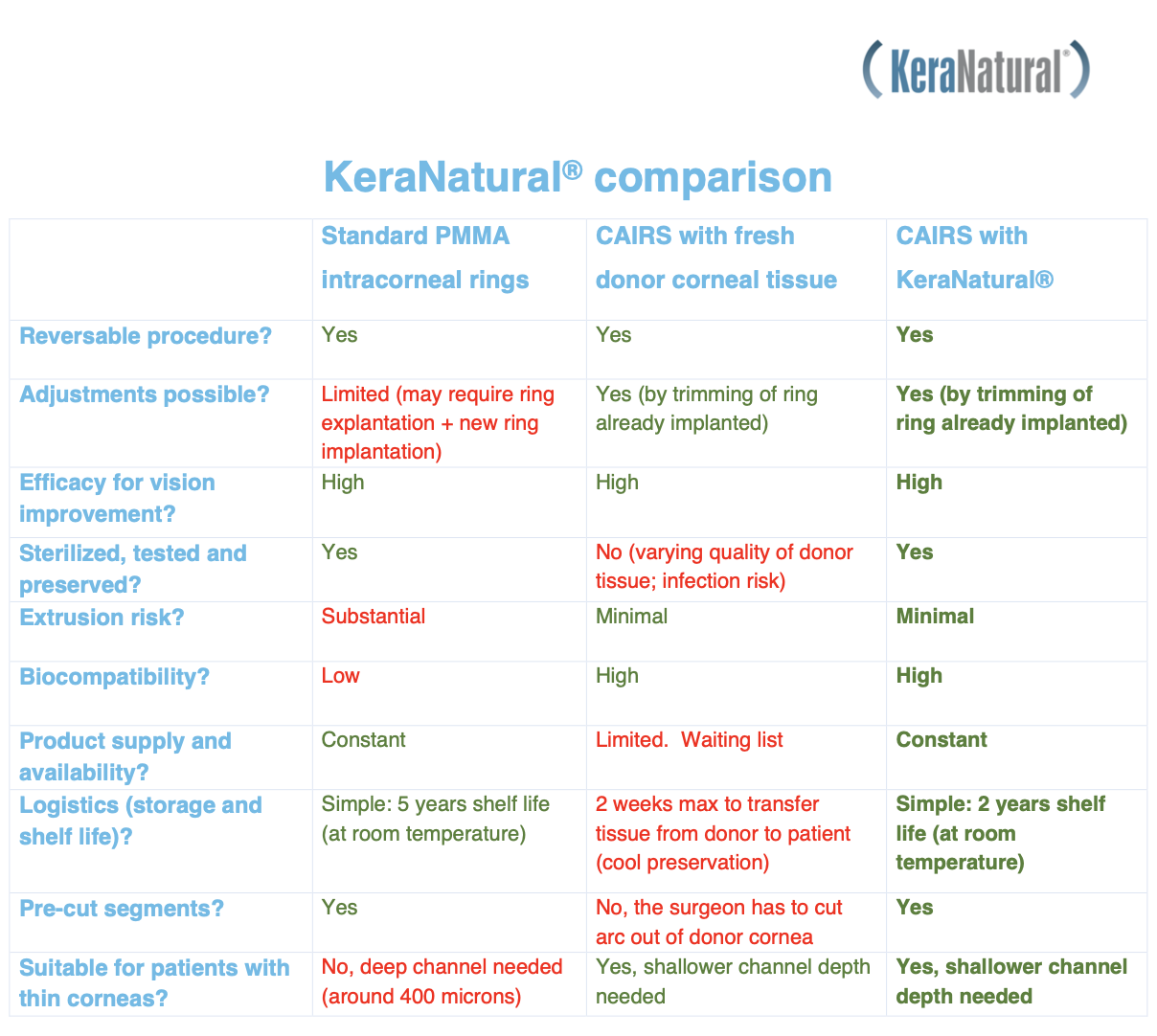
KeraNatural and traditional corneal rings are two different treatments for keratoconus and the main difference between them is in the materials they use to reshape the cornea. KeraNatural involves injecting a natural, biocompatible substance made from human collagen into the cornea, while traditional corneal rings are made of a plastic material called PMMA (poly-methyl-meth-acrylate). Here are some of the differences between KeraNatural and traditional corneal rings:
Material:
• KeraNatural is made of a natural, biocompatible substance called human collagen, a protein already present in the human body. This substance is obtained from donated human corneal tissue and processed to remove possible contaminants.
• Traditional corneal rings, on the other hand, are made of PMMA, a durable and corrosion-resistant synthetic polymer material.
Biocompatibility:
• Because KeraNatural uses a substance that is already present in the human body, it is generally considered biocompatible, meaning it is unlikely to cause any adverse reactions or rejection by the body.
• The PMMA used in traditional corneal rings is also considered biocompatible, but there is a small risk of allergic reaction or infection or corneal melting due to its synthetic nature.
Effectiveness:
• Both KeraNatural and traditional corneal rings have been shown to be effective in improving vision and slowing down the progression of keratoconus in many patients. The effectiveness of each treatment may depend on the severity of the condition and individual patient factors.
KeraNatural is a surgical procedure that involves the placement of human collagen rings in the cornea of the eye to reshape and improve vision in patients with keratoconus, a condition that causes the cornea to become progressively thinner and more curved like a cone leading to visual impairment.
The main goal of this procedure is to improve visual acuity and reduce the need for glasses or contact lenses. However, it is important to note that not all patients may be able to completely eliminate the need for corrective lenses after surgery and in rare cases the vision may not improve or even reduce.
While the majority of patients experience a significant improvement in their vision, the extent to which they can reduce or eliminate the use of glasses or contact lenses may vary depending on individual factors such as the severity of keratoconus and the patient’s specific visual needs.
It is important to discuss your individual situation with your ophthalmologist to determine the best course of treatment for your specific needs and expectations.
KeraNatural may be suitable for keratoconus patients who use contact lenses to correct their vision. In fact, one of the common indications for ICRS is intolerance to contact lenses due to keratoconus or poor vision with contact lenses.
KeraNatural can help reduce the irregularities that cause vision problems in keratoconus by improving the shape and the thickness of the cornea. This in turn can lead to improved visual acuity and greater comfort in wearing contact lenses.
However, the suitability of KeraNatural for a patient with keratoconus who wears contact lenses will depend on several factors, including the severity and progression of keratoconus, the thickness of the cornea and the patient’s overall eye health.
It is important that keratoconus patients considering using KeraNatural undergo a comprehensive eye examination and consult with an ophthalmologist who specializes in the treatment of keratoconus. The ophthalmologist can assess the patient’s condition and determine whether KeraNatural is a suitable treatment option.
KeraNatural is a surgical procedure for keratoconus patients that involves the placement of corneal allogenic ring segments in the cornea for the purpose of reshaping it and improving the vision.
A patient’s suitability for this treatment depends on several factors, including the severity of keratoconus, the thickness and shape of the cornea, and the overall health of the eye.
In general, allograft corneal ring treatment may be suitable for patients with moderate keratoconus who have not responded to other treatments such as contact lenses or glasses. It may also be an option for patients who are not candidates for corneal transplant surgery.
However, the final decision on whether a patient is suitable for this treatment should be made by an ophthalmologist specializing in keratoconus management after a thorough evaluation of the patient’s eye health and condition.
Corneal cross-linking is a treatment for keratoconus, a condition in which the cornea (the transparent front part of the eye) becomes progressively thinner and protrudes outward in a cone shape, causing visual impairment and reduced vision.
The benefits of corneal cross-linking treatment include:
• Stopping progression: corneal cross-linking treatment uses riboflavin drops and ultraviolet light to strengthen the cornea’s collagen fibers, which slows or stops the progression of keratoconus.
• By stopping the progression of keratoconus, corneal cross-linking can prevent the need for a corneal transplant (a surgical procedure that replaces the entire cornea with a donor cornea).
• Stabilisation of vision: in some cases corneal cross-linking can improve visual acuity by flattening the cornea and by reducing irregularities that cause visual distortion, however in most cases visual acuity does not change significantly.
• Minimal side effects: side effects of corneal cross-linking treatment are usually mild and temporary and include discomfort, light sensitivity and blurred vision. Serious complications are rare.
• Overall, corneal cross-linking is a safe and effective treatment for keratoconus and can help maintaining visual function while eliminating the need for more invasive procedures. It is important to note that not all patients with keratoconus may be suitable for corneal cross-linking and that a thorough eye examination and consultation with an ophthalmologist is necessary to determine the most appropriate treatment plan.
Table and some of this page elements have been taken with permission from Swiss Vision Group and modified.
Dr Borasio only receives at:
EYE PRO
Studio Oculistico
Via Carlo Giordana 5, Torino, Italy
Tel: +39 392 7231024
dr@edmondoborasio.com
About Dr Borasio
Curriculum VitaeFor professionals
PC Software for OphthalmologistsiOS Apps for OphthalmologistsPost LASIK Biometry ConsultationProcedures
Laser Vision CorrectionLaser Cataract SurgeryClear Lens Exchange
Presbyopia correction
Astigmatism Correction
Multifocal IOLs
ICL Phakic lens implantationKeratoconus management
Corneal Transplantation
Pterygium excision
Iris reconstruction
Intravitreal Injections (aVEGF)YAG laser capsulotomyYAG laser iridotomyYAG laser vitreolysis (floaters)SLT laser (glaucoma)Argon laser (retina)

